What is pneumococcus?
Streptococcus pneumoniae, also known as pneumococcus, is a bacterium that primarily affects infants, toddlers and the elderly. Pneumococcus can cause several types of infections, the most severe of which are called Invasive Pneumococcal Disease (IPD). IPD includes pneumonia (lung infection), meningitis (infection of the lining surrounding the brain and spinal cord), bacteremia (blood stream infection), septic arthritis (joint infections) and osteomyelitis (bone infections). Milder infections include ear infections and sinus infections.
In addition to chest pain, cough, fever, chills and difficulty breathing, pneumococcal pneumonia can cause lung abscesses, infection around the lungs, infection in the chest cavity, and/or inflammation of the lining of the heart. About 1 in 20 people with pneumococcal pneumonia die.
Pneumococcal meningitis has different symptoms depending on age. Older children and adults develop confusion, fever, headache, stiff neck and sensitivity to light. In babies, meningitis can cause extreme fussiness, vomiting, lethargy and poor eating or drinking. About 1 in 12 children who get pneumococcal meningitis will die. For those who survive, about one third will have long-term complications such as hearing loss and neurologic impairment. Such complications are more common in pneumococcal meningitis than in other forms of bacterial meningitis.
Pneumococcal bacteremia causes chills, fever and lethargy. It kills 1 in 30 children who develop it. Those who survive may require limb amputation due to poor circulation during the body’s inflammation response, called sepsis.
Children who are younger than 5 years old have an increased risk of IPD, with additional risk in those who attend daycare. This increased risk is due to the fact that infants and children cannot easily develop antibodies to the sugar (polysaccharide) that coats the bacteria.
Chronic medical conditions can also increase risk. Examples include heart, liver, kidney or lung disease, diabetes, sickle cell disease, a weakened immune system, poorly functioning or absent spleen, or a cochlear implant.
How is pneumococcus spread?
Pneumococcus is found in the lining of the nose and back of the throat in about 1 in 4 people. This is called colonization. People colonized with pneumococcus are typically older children and adults. Colonization does not make them sick because they have developed immunity through prior infection and/or vaccination. Respiratory secretions (e.g. saliva and mucous) of infected or colonized individuals contain pneumococcus and are spread by coughing, sneezing, or touching surfaces after eating or wiping the nose.
Because most mothers are immune to pneumococcus, their newborns will receive passive immunity in utero through the placenta. However, these maternal antibodies transferred to the baby only last a few months. This is why vaccination is recommended starting at age 2 months.
Infants and children are also at risk of IPD as a complication of influenza. When the respiratory tract is attacked by influenza, it provides the opportunity for pneumococcus to invade the body more deeply such as into the bloodstream, lungs or brain.
How common was pneumococcus prior to the vaccine?
Prior to the vaccine, pneumococcus caused about 700 cases of meningitis, 17,000 cases of bacteremia, 200 deaths and 5 million ear infections in children each year.
When and how was the pneumococcal vaccine developed?
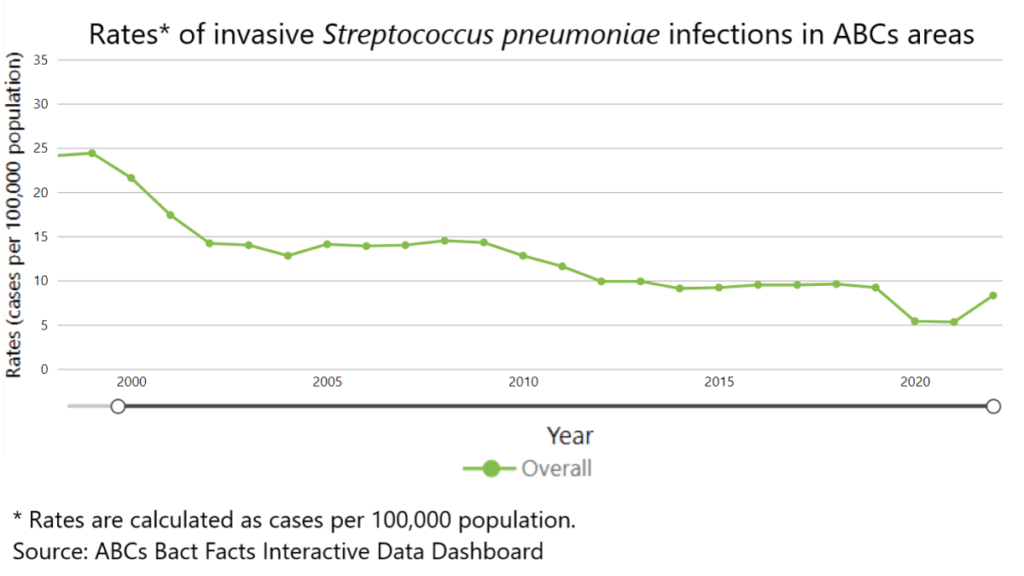
The pneumococcal vaccine was designed to primarily reduce pneumococcal meningitis and bacteremia. These are the two types of pneumococcal disease that are part of the CDC’s National Notifiable Diseases Surveillance System (NNDSS). This data is reported weekly. Surveillance of IPD began in 1998.
There are two types of pneumococcal vaccines: Polysaccharide vaccines (PPSV) and conjugate vaccines (PCV). PPSV protects against 23 subtypes of pneumococcus and is used in adults 65 and older and other adults who are considered high risk. Children do not develop good immunity with the polysaccharide vaccines so they instead receive PCV.
As described in some of our previous vaccine blogs, conjugate vaccines are made by using the pneumococcal polysaccharides (small sugars on the bacterial surface) and connecting (or conjugating) it to a harmless protein. When the child’s immune system responds to the harmless protein, it also triggers an immune response to the polysaccharides, thereby developing immunity against pneumococcus. Conjugate pneumococcal vaccines also reduce colonization in the person’s nose and throat. Therefore, vaccination against pneumococcus not only provides immunity but also reduction and colonization and spread.
The first vaccine was introduced for adults in 1977. The first PCV vaccine was FDA approved in 2000 and protected against 7 subtypes (i.e. strains) of pneumococcus. In 2010, PCV13 was FDA approved for children. PCV15 followed in 2022 and PCV20 in 2023. Each number after PCV, defines the number of pneumococcal strains protected against by the vaccine. For example, PCV20 contains 20 subtypes. PCV20 is the vaccine currently recommended for routine vaccination.
How much impact has pneumococcal vaccination had?
Thanks to pneumococcal vaccines, cases of IPD in children less than 5 years old went down by 95% from 1998 to 2021. IPD caused by the strains in PCV13 decreased by 99% over that same time. A gap in vaccination rates during the COVID-19 pandemic resulting in a slight in an increase in IPD cases between 2021 and 2022.
In addition to reducing IPD, the vaccine also helps with antibiotic resistance. In the 1940’s, all the strains of pneumococcus could be treated with penicillin. Now, many strains of pneumococcus are not only resistant to penicillin but several other antibiotics. Many parents can probably relate to amoxicillin not working for ear infections. Or multiple ear infection antibiotics failing, and us having to give painful antibiotic shots in their child’s legs. When pneumococcal infections are decreased by vaccine, there are fewer oral antibiotics prescribed, and fewer opportunities for the bacteria to be exposed to and develop resistance to antibiotics.
If my child got all their PCV vaccines, why did they still get ear infections?
Though pneumococcus is a leading cause of ear infections in children, it is not the only one. Additionally, even PCV20 does not protect against all the possible pneumococcal strains. So, ear infections still occur as a result of viruses, non-pneumococcal bacteria, or pneumococcal strains not covered by the vaccine. It is estimated that PCV prevents between 6 and 15 of every 100 ear infections caused by pneumococcus.
When do children receive the pneumococcal vaccine?
All children less than 5 years old and children 5-18 years old with certain risk conditions should receive the pneumococcal vaccine.
- Infants and young children usually need 4 doses of PCV to build their immune system to protective levels. These doses are recommended at 2, 4, 6, and 12–15 months of age.
- Older children and adolescents who did not receive the recommended doses as infants or young children may need PCV. This depends on age, underlying medical conditions, or other risk factors.
What are the possible side effects of the pneumococcal vaccine?
Most children who get a pneumococcal vaccine don’t have any serious side effects. The most common side effects are listed below.
- Pain or swelling at the site
- Decreased appetite
- Irritability
- Headache of muscle soreness
- Low grade fever (a few may develop a higher fever of 102 or more)
- Fatigue
More serious side effects such as anaphylaxis (severe allergic reaction) can occur but are exceedingly rare.
When comparing the risk of the vaccine to the risk of IPD, the risk of common, mild vaccine side effects is minimal compared to the risk of the disease and the complications associated with IPD.
What impact has the pneumococcal vaccine had on the incidence of pneumococcal disease around the world?
The World Health Organization (WHO) estimates that each year pneumococcus kills about 300,000 children under 5 worldwide – mostly in developing countries where the vaccine is not readily available. Pneumococcus is the leading cause of death from bacterial pneumonia globally; most of those deaths occur in Africa and Asia. Organizations that have helped countries introduce PCV into their national immunization programs have seen large reductions in IPD.
If pneumococcal infections have decreased, why does my child still need the vaccine?
Unfortunately, unlike some infections like polio, pneumococcal disease cannot be eradicated. There are more than 100 subtypes of pneumococcus so surviving one pneumococcal infection does not preclude you from contracting disease from another strain. Until children get older and their immune systems mature, vaccination is the best way to continue to protect them. As shown in the chart below, when vaccination rates decrease (in this case due to the COVID-19 pandemic), PID rates increase.
References
2024. “Streptococcus pneumoniae (Pneumococcal) Infections266 “, Red Book: 2024–2027 Report of the Committee on Infectious Diseases, Committee on Infectious Diseases, American Academy of Pediatrics, David W. Kimberlin, MD, FAAP, Ritu Banerjee, MD, PhD, FAAP, Elizabeth D. Barnett, MD, FAAP, Ruth Lynfield, MD, FAAP, Mark H. Sawyer, MD, FAAP
https://www.chop.edu/vaccine-education-center/vaccine-details/pneumococcal-vaccine
https://www.meningitis.org/meningitis/bacterial-meningitis/pneumococcal-meningitis
https://www.immunize.org/ask-experts/what-are-the-recommendations-for-pneumococcal-vaccination-of-children-and-adults/https://www.cdc.gov/pneumococcal/php/surveillance/index.html