What is HPV?
HPV, or human papillomavirus, is a small DNA virus. There are two types of HPV: cutaneous and mucosal. Cutaneous HPV can cause pesky warts on the skin, typically of the extremities. Mucosal HPV can cause warts of the eyes, nose, mouth, throat, genitals and anus. Most mucosal HPV infections will resolve on their own in 12 months without treatment. Those that do not have a higher risk of causing pre-cancerous or cancerous lesions. Because the HPV vaccine is for mucosal HPV prevention, the remainder of this blog will focus solely on this type.
How is HPV spread?
Mucosal HPV is spread through contact of mucosal surfaces which are the moist linings of various body parts such as the inside of eyelids, inside of lips, mouth, throat, respiratory tract, gastrointestinal tract, anus and genitals. Mucosal contact typically occurs through vaginal intercourse, but could also include oral or anal sex, or non-intercourse contact of genitals. Mucosal HPV has also been documented being transmitted from mother to infant’s respiratory tract during childbirth.
How common are HPV infections?
Mucosal HPV is the most common sexually transmitted infection in the U.S. and worldwide, infecting 3 out of every 4 adults by the time they are 30 years old. Every year about 13 million Americans are newly infected with HPV. Between 35,000 and 45,000 U.S. men and women develop HPV-caused cancers each year. There are approximately 7,000 deaths annually in the U.S. due to HPV-caused cancers.
Can HPV be treated?
Unfortunately, there is no anti-viral medicine for HPV. Genital warts can be treated with topical agents, frozen, or removed with surgical or laser therapy. Cancerous HPV lesions are removed with surgery and may also require radiation and/or chemotherapy.
What type of vaccine is the HPV vaccine?
Gardasil® is a recombinant protein vaccine. A unique surface protein from each of 9 different wart and cancer-causing HPV strains is grown in yeast cells, then packaged in the vaccine vehicle for administration. The vaccine contains no live virus or HPV genetic material (i.e. DNA). The vaccine cannot cause HPV infections. Gardasil® is the only HPV vaccine distributed in U.S. Other HPV vaccines include CervarixTM, which only protects against strains 16 and 18 and is available in Europe, and the first generation Gardasil®vaccine that protected against only 4 strains (6, 11, 16 and 18).
What is the benefit of vaccinating against HPV?
Only two of the routine vaccines administered in the United States are cancer-preventing vaccines: hepatitis B and HPV. Gardasil® protects against the 9 different HPV strains most associated with genital warts and cancers. Two of the strains (6 and 11) cause approximately 90% of genital warts cases. The other 7 HPV strains for which Gardasil® provides protection are responsible for 90% of cervical cancers. Two of these other 7 strains (16 and 18) cause 70% of all cervical cancers, 60% of HPV-positive vaginal cancers, up to 75% of HPV-positive vulvar cancers, and 90% of all anal cancers.
How effective is the HPV vaccine?
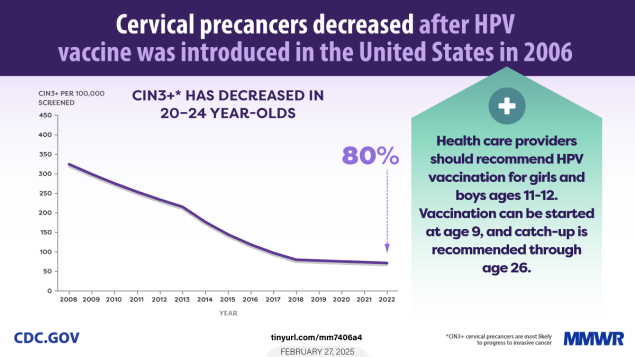
Over 97% of people develop antibodies to HPV after vaccination. This degree of immune response has led to some remarkable trends in cervical precancer, cancer and cancer death rates over the last 20 years.
A study published in JAMA in November 2024 monitored cervical cancer deaths among women younger than 25 years old. It found a remarkable decline between 2016-2021 amongst the first women protected by the HPV vaccine. The study showed a yearly 15% decrease in cervical cancer mortality starting in 2013 through 2021 with an overall reduction in cervical cancer deaths by 62%.
A CDC report from February 27, 2025 found an 80% reduction in cervical precancer lesions among women aged 20-24 years old screened between 2008 and 2022.
When should the vaccine be administered?
HPV vaccines are recommended to be administered starting at age 11 (though FDA approved down to age 9). Follow up studies on HPV vaccines over the last two decades have shown that young people who receive their first dose prior to turning 15 years old make a stronger immune response, and require only 2 doses. Those 15 and older require a 3-dose series for adequate protection. Because the vaccine does not work against current infections, early vaccination also allows time for the immune system to develop antibodies against the virus well before any possible exposure. As with all vaccines, protection before exposure is key! Women in the original clinical trials continue to show robust antibody levels 20+ years later in follow-up studies.
Is the vaccine safe?
Yes! Over 135 million doses of the vaccine have been administered in the United States with no serious safety concerns. Monitoring continues in over 80 countries. Common side effects of the vaccine include pain and redness at injection site. The vaccine can sometimes make preteens and adolescents feel lightheaded during or after administration (as many medical procedures can). We have patients remain in the office for 10-15 minutes after administration to monitor for this side effect.
Isn’t the HPV a new vaccine? Do we have long-term safety and effectiveness data?
The original 4-strain (6,11,16,18) version of Gardasil® was FDA approved in 2006. The current 9-strain version was FDA approved in 2014. Many mothers of PAR patients have told us they participated in the clinical trials in the early 2000s (to those who did, thank you for your contribution to our understanding of this virus and its vaccine!). Relative to the polio vaccine, which was first introduced in 1955, HPV vaccines are new. But we have nearly 20 years of ongoing effectiveness and safety data from which we base our recommendations to protect against HPV-related cancers through vaccination. So, no, this is not a “new vaccine” anymore.
If my son can’t get cervical cancer, why should he get the HPV vaccine?
Though men cannot get cervical cancer, there are HPV-related cancers they can get: penile, anal, mouth, throat. The dramatic drop in cervical cancer rates in the 21st century due to HPV vaccination, screening, early detection and treatment have resulted in male HPV cancers now making up about 40% of new diagnoses (~16,000 U.S. men) each year. Additionally, by vaccinating both men and women, we have the potential to stop the spread of mucosal HPV completely. Doing so could eradicate genital warts and many HPV-caused cancers.
I’m raising my child to wait until marriage to have sex, so why should I vaccinate them?
We never know who our children will fall in love with. At the time they fall in love, their significant other may share the same values but may have been exposed in years prior. If we have a safe way to protect against the unexpected for our child, and a potential cancer diagnosis is at stake, the benefit outweighs the low risk of side effects. Many people are fortunate enough to go through life and never be in a car accident, but that doesn’t mean they shouldn’t wear their seatbelt just in case.
Will getting a vaccine against a sexually transmitted infection cause my child to feel free to be more sexually promiscuous?
No, multiple papers have analyzed cohorts in many different countries and have shown no differences in pregnancies, sexually transmitted infections, age at first sexual experience, number of sexual partners, or use of condoms in young women who had received HPV vaccination vs. those who had not.
References:
2024. “Human Papillomaviruses”, Red Book: 2024–2027 Report of the Committee on Infectious Diseases, Committee on Infectious Diseases, American Academy of Pediatrics, David W. Kimberlin, MD, FAAP, Ritu Banerjee, MD, PhD, FAAP, Elizabeth D. Barnett, MD, FAAP, Ruth Lynfield, MD, FAAP, Mark H. Sawyer, MD, FAAP
HPV: Facts About the Virus that Causes Cancer and How to Prevent It. (n.d.). HealthyChildren.org. https://www.healthychildren.org/English/safety-prevention/immunizations/Pages/are-your-kids-protected-from-cancer-caused-by-hpv.aspx
https://www.cdc.gov/hpv/about/index.html
https://www.chop.edu/vaccine-education-center/vaccine-details/human-papillomavirus-vaccine
Ogilvie GS, Phan F, Pedersen HN, Dobson SR, Naus M, Saewyc EM. Population-level sexual behaviours in adolescent girls before and after introduction of the human papillomavirus vaccine (2003-2013). CMAJ. 2018 Oct 15;190(41):E1221-E1226. doi: 10.1503/cmaj.180628. PMID: 30322986; PMCID: PMC6188947.
Dorali P, Damgacioglu H, Clarke MA, Wentzensen N, Orr BC, Sonawane K, Deshmukh AA. Cervical Cancer Mortality Among US Women Younger Than 25 Years, 1992-2021. JAMA. 2025 Jan 14;333(2):165-166. doi: 10.1001/jama.2024.22169. PMID: 39602175; PMCID: PMC11733696.
Gargano JW, Stefanos R, Dahl RM, et al. Trends in Cervical Precancers Identified Through Population-Based Surveillance — Human Papillomavirus Vaccine Impact Monitoring Project, Five Sites, United States, 2008–2022. MMWR Morb Mortal Wkly Rep 2025;74:96–101. DOI: http://dx.doi.org/10.15585/mmwr.mm7406a4
Leidner AJ, Chesson HW, Talih M. HPV vaccine status and sexual behavior among young sexually-active women in the US: evidence from the National Health and Nutrition Examination Survey, 2007-2014. Health Econ Policy Law. 2020 Oct;15(4):477-495. doi: 10.1017/S1744133119000136. Epub 2019 May 21. PMID: 31109388; PMCID: PMC6868297.
Donken R, Ogilvie GS, Bettinger JA, Sadarangani M, Goldman RD. Effect of human papillomavirus vaccination on sexual behaviour among young females. Can Fam Physician. 2018 Jul;64(7):509-513. PMID: 30002026; PMCID: PMC6042675.